Yes Virginia, there are two ways of treating pain in this world. Pill versus no pill. And where do I stand on this?
Obviously I am partial to no-pain-pill approach or I’d be out of a job as a Physical Therapist if pain management rely on drugs alone. It’s undeniable, however, there are conditions when pain pill is necessary. Surgery is one. Or Cancer. Or toothache. Or hospice care. Or palliative care. These are conditions that will make someone suffer immensely without some form of medication. I will be dealing with very angry, screaming, crying, uncooperative patients who are deprived of legitimate pain meds. It can be human abuse and cruelty in fact, if that is the case.
Pain pills depend on the stage of the condition. Acute pain is that period immediately after an injury or malady onward to its resolution. Usually administration of pain should be tapered off as the full recovery is approached. Chronic pain lingers beyond 90 days and the sufferer begins to ask for more doses. Weaning is a hellish nightmare for them. We are talking of addiction. And addiction can have devastating consequences. Let us review some actions and side effects of most common pain meds:
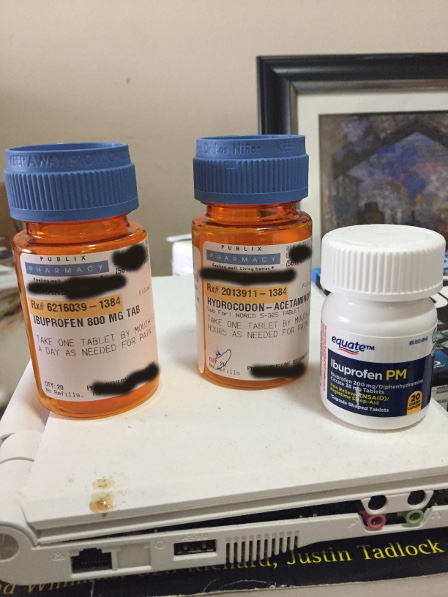
NSAIDS such as ibuprofen (Advil, Motrin) can lead to heart problems in prolonged use. It is worse with Diclofenac (Voltaren). These medications block cyclo-oxiganase(COX2) enzymes that cause pain and inflammation due to overproduction of prostaglandins. Problem is, the inhibition of COX2 is known also to cause stomach problems, indigestion and heart conditions. They also have the ‘ceiling effect’. That means no matter how much dosage you increase the medication, the pain relief will stay the same but the side effects increase. To those who take these mostly over the counter pain pills, please start weaning as soon as possible and try other pain relieving approaches: movement is the best approach. Yoga, meditation, music, heat packs, massage, psychotherapy, PT (of course) are very useful. Better yet, keep moving, nothing can beat movement in the prevention and relief of pain.
Opioids, i.e. Morphine, Oxycodone, Methadone, Codeine are narcotics that can become addictive. Overdosage can lead to respiratory distress, hypotension, dreaded constipation, bowel obstruction, ileus. Opioids work by targeting the root cause of pain in the brain and they don’t have ‘ceiling effect’ which means the higher the dosage, the lesser the pain symptoms (improved analgesic effects). In other words, people can develop high tolerance to these meds which may require higher dosages in future. And that can lead to addiction. It becomes more dangerous when withdrawn - leading to drug withdrawal symptoms. The side-effects alone are enough to frighten anyone using these meds. And though some people legitimately need them at least during the acute phase of their painful conditions, it is imperative to be very vigilant in dosages and time-frame of use. I have had patients who became instant ‘drug-addict suspects’ when they knew more about pain meds than pharmacists :) or when the intensity of their pain is a 10 while laughing or having a pleasant conversation over the phone. Yup - I have no right to treat them differently from my other patients but one should be careful in over-prescribing with inconsistent or non-reliable symptoms. And these are not only limited to patients. They could also be friends and family members. Prescribing pain pills is outside the scope of my practice but these patients should immediately be referred to Pain Management professionals before it’s too late.
Finally, there are drugs that can ‘harness’ the impact of a pain pill. They are antidepressants, anticonvulsants, local anesthetics and corticosteroids. Together with opioids, they provide a maximum analgesic effect. These ‘harnessing’ drugs have side-effects of their own combined with pain meds. Mostly drowsiness, irritability, slow movements and in case of corticosteroids - kidney and liver side-effects.
There are always legitimate conditions that require pain pills. Unfortunately, the current trend points to their overuse and the victims mostly likely did not intend to become drug dependent in the first place. Someone does not wake up in the morning with that goal in mind. The most likely scenario is that he had a pain he needed to address. Temporarily. But the pain becomes chronic (about 90 days) and only the prescription with increased dosage (ceiling effect) would help him make it through each day. When he tries to wean himself off it, he goes through withdrawal. In no time, he would revert back to it to avoid the withdrawal symptoms. The cycle continues. That is addiction.
That prescription pill addict could be me or you or someone we both know, or a parent, sibling, friend co-worker. Pain does not discriminate and there are situations and environments that render one person more susceptible to pain than another.
[The following is copied from PT in Motion] Here are some statistics via The Centers for Disease Control and Prevention (CDC), which released guidelines in March 2016 encouraging health care providers to try safer alternatives like physical therapy for most pain management:
1. In 2012, health care providers wrote 259 million prescriptions for opioid pain medication, enough for every American adult to have their own bottle of pills.
2. As many as 1 in 4 people who receive prescription opioids long term for noncancer pain in primary care settings struggles with addiction.
3. Sales of prescription opioids have nearly quadrupled since 1999.
4. Deaths related to prescription opioids have quadrupled.
5. Heroin-related overdose deaths more than quadrupled between 2002 and 2014, and people addicted to prescription opioids are 40 times more likely to be addicted to heroin.
6. More than 165,000 persons in the United States have died from opioid pain-medication-related overdoses since 1999.
7. Every day, more than 1,000 people are treated in emergency departments for misusing prescription opioids.